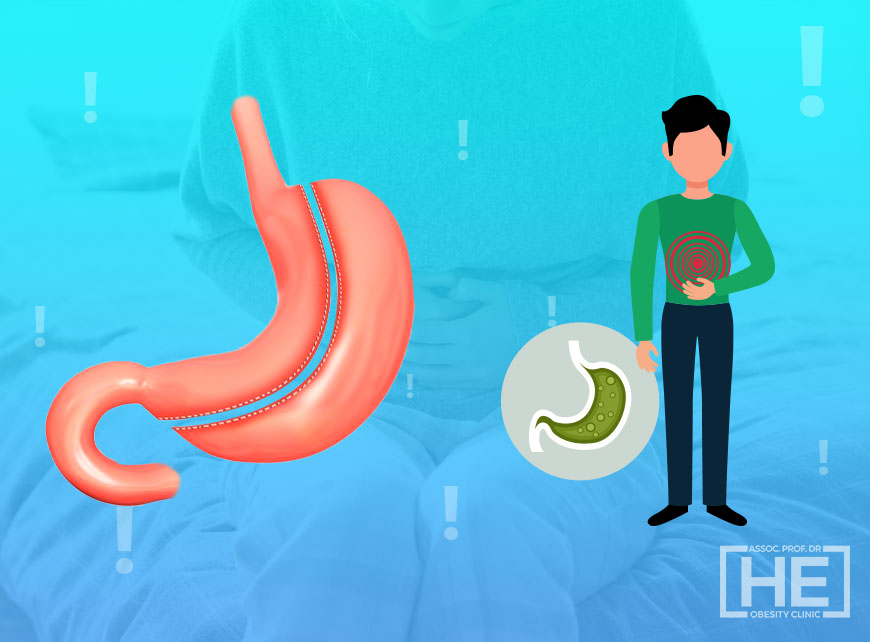
Acid reflux after gastric sleeve, signs of acid reflux after gastric sleeve surgery, What helps with acid reflux after gastric sleeve? What causes acid reflux after gastric sleeve? How to stop acid reflux after gastric sleeve? What can i take for acid reflux after gastric sleeve? How to get rid of acid reflux after gastric sleeve? What causes severe acid reflux after gastric sleeve? Is acid reflux normal after gastric sleeve? Acid reflux is one of the most important problems after obesity surgery. Patients who have undergone bariatric surgery may be admitted to the emergency department with severe epigastric pain, a burning pain in the chest, or chest pain.
Gastric sleeve surgery, also known as sleeve gastrectomy, is a popular and effective weight loss procedure that involves removing a large portion of the stomach to reduce its size and capacity. While the surgery has been proven to help patients achieve significant weight loss and improve obesity-related health conditions, such as diabetes and high blood pressure, some patients may experience acid reflux after the procedure.
Severe gastroesophageal combustion can occur at a rate as high as 47%. This condition is often associated with reflux disease, which is skipped before obesity surgery. If a complete dissection of the left hiatal dry is not performed during surgery, it is also extremely easy to skip a concomitant hiatus hernia.
With current scientific data, the issue of reflux after tube stomach surgery is somewhat contradictory. But one thing we do know is that the most important complication that badly affects the quality of life of patients after tube stomach surgery is reflux and stomach hernia.
It changes more dramatically after Gastric sleeve surgeries. Removal of the fundus and body of the stomach affects gastric harmony and acid secretion. These anatomical and physiological changes create a new balance between the enhancing and protective factors for reflux disease.
Aggressive dissection and closure of the hiatal defect are very important for hiatal hernia during surgery. The appearance of reflux symptoms after sleeve gastrectomy usually occurs in the first postoperative year.
The second peak of reflux may be in the later period and may be due to the formation of neofundus. This, in turn, is mostly caused by incomplete resection of the fundus in the first operation.
What is Acid Reflux?
Acid reflux disease can simply be described as the formation of damage to the layer covering the esophagus due to acid and bile as a result of the escape of stomach contents into the esophagus.
Acid reflux, also known as gastroesophageal reflux disease (GERD), occurs when the stomach acid flows back into the esophagus, causing a burning sensation in the chest or throat. This can lead to symptoms such as heartburn, regurgitation, chest pain, difficulty swallowing, and coughing. While occasional acid reflux is common and can be managed with over-the-counter medications and lifestyle changes, persistent or severe acid reflux can have a significant impact on a patient’s quality of life.
In this case, two things can happen, either the event is temporary, or the patient receives treatment and the epithelial tissue regenerates, or if the damage is chronic, the epithelial here changes to withstand acid, meaning it tries to resemble the tissue lining the inside of the stomach.
This situation is dangerous. This transformation, called the Barrett’s esophagus, is considered a precursor to esophageal cancers in the long term if it continues.
One of the factors that causes reflux disease is impaired movement in the esophagus. In studies, approximately 40% of obese patients have an esophageal movement disorder. The most common is nonspecific movement disorder.
This is followed by the nutcracker esophagus. The pressure of the lower esophageal cap is between 10-35 mmHg. In studies, it is seen that the pressure of the lower esophageal valve decreases as the body mass index increases.
This, in turn, is one of the factors that prepare the basis for stomach reflux. The incidence of hiatal hernia in obese patients is much higher than in the normal population. This, in turn, increases the incidence of reflux and, with it, esophagitis in this group of patients.
Acid Reflux After Gastric Sleeve Surgery
Gastric sleeve surgery, also known as sleeve gastrectomy, is a surgical weight-loss procedure in which the stomach is reduced to about 15% of its original size, resulting in a sleeve-shaped stomach. This procedure has gained popularity as an effective treatment for obesity and related health issues. While gastric sleeve surgery has been successful for many individuals in achieving significant weight loss and improving overall health, some patients may experience acid reflux after the procedure.
Acid reflux, also known as gastroesophageal reflux disease (GERD), is a condition in which stomach acid flows back into the esophagus, causing discomfort and potential damage to the esophageal lining. Symptoms of acid reflux may include heartburn, regurgitation of food or sour liquid, difficulty swallowing, and chest pain. If left untreated, acid reflux can lead to more serious complications such as esophagitis, esophageal strictures, and Barrett’s esophagus.
The relationship between gastric sleeve surgery and acid reflux is complex and not fully understood. However, there are several factors that may contribute to the development or exacerbation of acid reflux following gastric sleeve surgery.
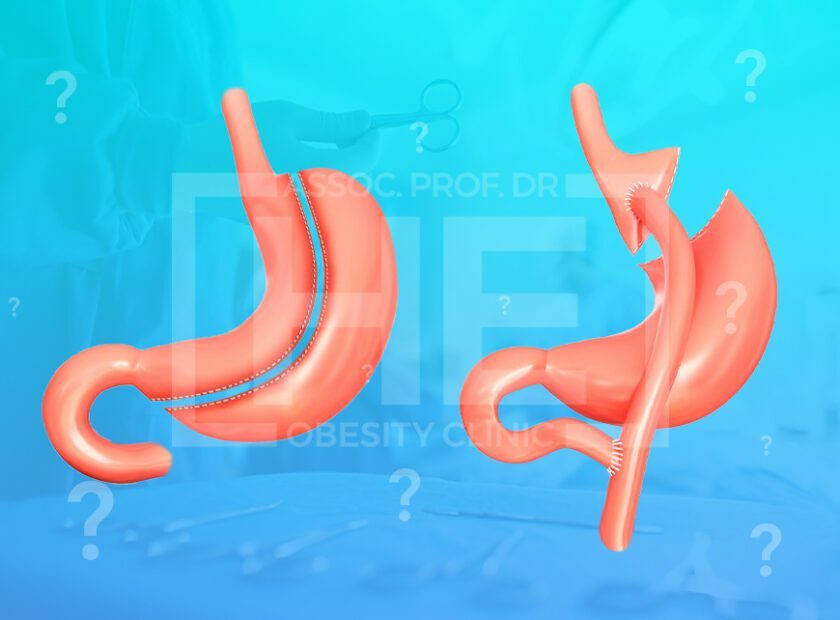
One potential factor is the alteration of the stomach’s anatomy. During gastric sleeve surgery, a portion of the stomach is removed, including the fundus, which is the upper part of the stomach that produces ghrelin, a hormone associated with hunger. This anatomical change can affect the function of the lower esophageal sphincter (LES), the muscle that separates the esophagus from the stomach and helps prevent acid reflux. Disruption of the normal anatomy and function of the LES can lead to an increased risk of acid reflux.
Another factor that may contribute to post-operative acid reflux is the rapid weight loss experienced by patients after gastric sleeve surgery. Significant weight loss can lead to changes in body composition, including a reduction in adipose tissue and changes in hormone levels. These changes can affect the function of the LES and increase the likelihood of acid reflux.
In addition to anatomical and physiological factors, dietary and lifestyle habits can also play a role in the development of acid reflux after gastric sleeve surgery. Patients may be advised to follow a specific diet after surgery, which typically involves consuming smaller portion sizes and avoiding certain foods that are known to trigger acid reflux, such as spicy foods, citrus fruits, and caffeine. However, adherence to dietary recommendations may vary among patients, and poor dietary choices or overeating can contribute to the development of acid reflux.
Management of acid reflux after gastric sleeve surgery involves a comprehensive approach that addresses both lifestyle modifications and medical interventions. Patients who experience symptoms of acid reflux should consult with their healthcare provider to determine the most appropriate course of action.
Lifestyle modifications may include:
– Eating smaller, more frequent meals
– Avoiding lying down or going to bed immediately after eating
– Elevating the head of the bed while sleeping
– Identifying and avoiding trigger foods
– Maintaining a healthy weight through regular physical activity
In addition to lifestyle modifications, medical interventions may be necessary to manage acid reflux after gastric sleeve surgery. These interventions may include:
– Proton pump inhibitors (PPIs) or H2-receptor antagonists to reduce stomach acid production
– Prokinetic agents to improve gastrointestinal motility
– Surgical revision procedures to address anatomical issues contributing to acid reflux
What Helps With Acid Reflux After Gastric Sleeve?
Causes of Acid Reflux After Gastric Sleeve Surgery
Acid Reflux After Gastric Sleeve Surgery Management and Treatment
Acid Reflux After Gastric Sleeve Surgery Prevention
Acid Reflux and Gastric Sleeve Surgery
Like all obesity surgeries, a rapid weight loss occurs after Gastric Sleeve Surgery, and serious improvements in diabetes, blood pressure, asthma, COPD and many other metabolic diseases are observed in this process.
According to the studies of hormones like leptin also decreased in white adipose tissue in the body that is the result of a decline enflamatuar retracted condition of the breast, colon, pancreatic, ovarian, and other cancers have an increased risk of leads to a decrease in shows.
All bariatric surgery patients should be subjected to preoperative endoscopy. Patients with severe reflux or Barrett’s esophagus should definitely not undergo tube stomach surgery. After tube stomach surgery, endoscopic control should be performed at the end of 1 year.
According to the results of this endoscopy and the patient’s complaints, the results of the biopsy should be followed up regularly or treated with radiofrequency therapy. In patients with a lot of damage due to reflux or who develop dysplasia, an overhaul should be performed urgently with Roux-en-Y gastric bypass surgery.
In those who do not have reflux disease, there is no obstacle in terms of tube stomach surgery. In patients with mild reflux complaints, it has been shown in studies that a gastric valve narrowing operation called cruroaphy should be added together with tube stomach surgery, but even in patients with cruroaphy in the long term, there is a high risk of re-developing reflux complaints. Patients need to be aware of this risk.
Finally, the complaints of severe Esophagitis and severe reflux of the stomach tube before surgery in patients with these complaints have been for the last 1-2 years that can progress very often yet to reveal the precise recommendations, but patients with severe reflux esophagitis patients with central obesity and this group was given to a joint decision with the patient after information is given, and then the tube outside of the stomach obesity surgery stomach surgery that should be offered to advocates and other derivative bypass pressure reducer.
What causes acid reflux after gastric sleeve?
Gastric sleeve surgery, the majority of the stomach is taken into a small tube, which reduces the volume in the stomach and increases the pressure.
If the stomach acid does not have much volume to accumulate, the pressure also increases, if the patient has a stomach hernia, that is, the stomach acid that goes back to the esophagus and comes into contact with the eating pipe leads to acid reflux disease and complaints.
Even in the group of obese patients who did not complain of stomach hernia or acid reflux before, it has been found in scientific research that acid reflux complaints may occur after the gastric sleeve.
In short, there is no obstacle in terms of gastric sleeve surgery in those who do not have gastric hernia/reflux disease.
In patients with mild reflux complaints, it has been shown in studies that gastric sleeve surgery should be added along with gastric sleeve surgery to narrow the gastric valve called cruroaphy, however, even in patients with cruroaphy in the long term, there is a high risk of re-developing reflux complaints. Patients need to be aware of this risk.
How common is acid reflux after gastric sleeve?
The problem of reflux is one of the most important problems after gastric sleeve surgery. In patients undergoing surgery, epigastric pain and severe chest pain may occur. Severe gastroesophageal burning can be observed as high as 47%.
This condition is often due to a reflux disease that is skipped before obesity surgery. If a complete dissection of the left hiatal course is not performed during the operation, it is also extremely easy to bypass an accompanying hiatal hernia.
After the operation, it changes more dramatically. Removal of the gastric fundus and its trunk affects gastric compliance and acid secretion. These anatomical and physiological changes create a new balance between the enhancing and protective factors for reflux disease.
Aggressive dissection and closure of the hiatal defect are very important for hiatal hernia during surgery. The appearance of reflux symptoms after sleeve gastrectomy usually occurs in the first postoperative year.
The second peak of reflux may be in a later period and may be due to the formation of a neofundus. This, in turn, is most often caused by incomplete resection of the fundus in the first operation.
Does acid reflux go away after gastric sleeve surgery?
Gastric sleeve operations are one of the safe and effective methods that can be applied to people who meet certain conditions. Obesity patients who complain of reflux can also have stomach reduction surgery.
A decrease in the volume of the stomach, food leaves the stomach faster, a decrease in the rate of acid by removing the fundus of the stomach, post-operative diet programs can help treat reflux. During surgery, the size of the stomach valve can also be rearranged.
In addition, a hernia of the stomach, which is very common with reflux and causes reflux, can also be treated with a surgical method called hiatal hernia during gastric sleeve surgery. This operation can prevent reflux complaints after surgery. But here is a very important point.
Gastric sleeve surgery is not recommended for people who complain of severe reflux. For this reason, before surgery, the patient should be examined in detail with or without complaints.
How can I fix my acid reflux after gastric sleeve surgery?
Reflux problem is one of the most important problems after gastric sleeve surgery. Patients with Gastric sleeve surgery may have epigastric pain or chest pain. The source of these problems is reflux disease.
Laparoscopic gastric sleeve surgery is preferred, ensuring that the natural structure of the digestive system and the passage traffic of foods are not changed and protected. In this way, vitamin and mineral deficiency is less common.
Another advantage is that because there is no by-pass here, dumping syndrome does not occur due to the natural progression of foods, especially due to the sudden transition of sugary foods to the small intestine. With this method, less reflux complaints are experienced in the stomach.
After this operation, a significant number of patients have enough reflux problems to require medication.
In some series, this frequency has been reported in one out of every 4 patients. Instead of gastric sleeve surgery in patients with severe reflux before surgery, other obesity surgeries should be recommended to patients.
If you do not want to experience reflux problems after surgery, you should act according to the doctor’s recommendations and recommended nutrition program.